 What is a Laparoscopic Bilateral Salpingo-Oophorectomy?
What is a Laparoscopic Bilateral Salpingo-Oophorectomy?
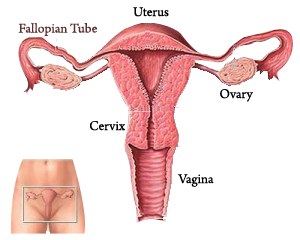
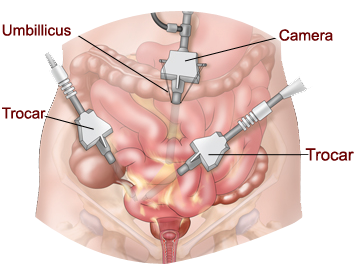
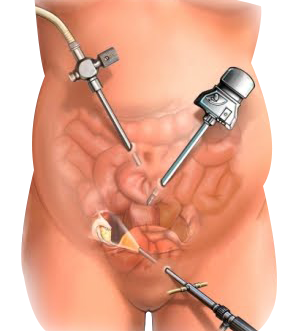
This is a surgery where your doctor uses a thin, lighted camera and small surgical tool placed through a small (1/2 inch) incision usually in the belly button, to remove both of your ovaries and fallopian tubes. To help with the surgery, two to three other small incisions will be made on the lower abdomen.
Why is this surgery used?
If you:
• are at high risk for ovarian cancer.
• have certain types of breast cancer.
• have certain types of ovarian masses or cysts.
How do I prepare for surgery?
• Before surgery, a pre-op appointment will be scheduled with your doctor at their office or with a nurse practitioner or physician assistant at Domino Farms.
• Depending on your health, we may ask you to see your primary doctor, a specialist, and/or an anesthesiologist to make sure you are healthy for surgery.
• The lab work for your surgery must be done at least 3 days before surgery.
• Some medications need to be stopped before the surgery. A list of medications will be provided at your pre-operative appointment.
• Smoking can affect your surgery and recovery. Smokers may have difficulty breathing during the surgery and tend to heal more slowly after
surgery. If you are a smoker, it is best to quit 6-8 weeks before surgery. If you are unable to stop smoking before surgery, your doctor can order a nicotine patch while you are in the hospital.
• You will be told at your pre-op visit whether you will need a bowel prep for your surgery and if you do, what type you will use. The prep to clean your bowel will have to be completed the night before your surgery.
• You will need to shower at home before surgery. Instructions will be provided at your pre-operative appointment.
• Do not wear makeup, nail polish, lotion, deodorant, or antiperspirant on the day of surgery.
• Remove all body piercings and acrylic nails.
• If you have a “Living Will” or an “Advance Directive”, bring a copy with you to the hospital on the day of surgery.
• Most women recover and are back to most activities in 1-2 weeks. You may need a family member or a friend to help with your day-to-day activities for a few days after surgery.
 What can I expect during the surgery?
What can I expect during the surgery?
• In the operating room, you will be given general anesthesia.
• After you are asleep and before the surgery starts:
• A tube to help you breathe will be placed in your throat.
• Another tube will be placed in your stomach to remove any gas or other contents to reduce the likelihood of injury during the surgery. The tube is usually removed before you wake up.
• A catheter will be inserted into your bladder to drain urine and to monitor the amount of urine coming out during surgery. The catheter will stay in until the next day.
• Compression stockings will be placed on your legs to prevent blood clots in your legs and lungs during surgery.
• After you are asleep the laparoscope is inserted into the abdomen and carbon dioxide gas is blown into the abdomen to inflate the belly wall away from the internal organs.
• Photographs may be taken during the surgery and will be placed in your medical records.
• Your ovaries and fallopian tubes will be sent to the lab where a pathologist will look at them under a microscope. The results of the lab tests should be available in about 1 week after surgery.
• If you have BRCA gene mutations, special lab test will be performed.
• When surgery is finished, a band-aid or small dressing will be placed over your incisions. You will wake up after the breathing tube is removed.
• The incision on your right side will be larger than others because your ovaries will be removed from that incision. You can expect to feel more discomfort on your right side for the first 2-3 weeks after surgery.
 What are possible risks from this surgery?
What are possible risks from this surgery?
Although there can be problems that result from surgery, we work very hard to make sure it is as safe as possible. However, problems can occur, even when things go as planned. You should be aware of these possible problems, how often they happen, and what will be done to correct them.
Possible risks during surgery include:
• Bleeding: If there is excessive bleeding, you will be given a blood transfusion unless you have personal or religious reasons for not wanting blood. This should be discussed with your doctor prior to the surgery.
• Damage to the bladder, ureters (the tubes that drain the kidneys into the bladder), and to the bowel: Damage occurs in less than 1% of surgeries. If there is damage to the bladder, ureters, or to the bowel they will be repaired while you are in surgery.
• Conversion to an open surgery requiring an up and down or Bikini incision: If a bigger open incision is needed during your surgery, you may need to stay in the hospital for one or two nights.
• Death: All surgeries have a risk of death. Some surgeries have a higher risk than others.
Possible risks that can occur days to weeks after surgery:
• A blood clot in the legs or lungs: Swelling or pain, shortness of breath, or chest pain are signs of blood clots. Call you doctor immediately if any of these occur.
• Bowel obstruction: A blockage in the bowel that results in not passing stool or gas. May cause stomach pain, bloating or vomiting.
• Hernia: Weakness in the muscle at the incision that causes a lump under the skin.
• Incision opens
• Infection: Bladder or surgical site infection. This may cause fever, redness, swelling or pain.
• Scar tissue: Tissue thicker than normal skin forms at the site of surgery.
What happens after the surgery?
• You will be taken to the recovery room and monitored for a short time before going home.
• You will be given medications for pain and nausea.
• You will have the compression stockings on your legs to improve circulation.
• You may have some vaginal spotting of bright red, brown, or black discharge.
• You may have cramping, feel bloated, or have shoulder pain.
• You may have a scratchy or sore throat from the tube used for your anesthesia.
• You will be given a small plastic device to help your breathing after your surgery at your bedside to help expand your lungs while you’re in bed.
• You will start walking as soon as possible after the surgery to help healing and recovery.
At Home After Surgery
If you use a bowel prep before surgery, it is common not to have a bowel movement for several days.
Call your doctor right away if you:
• develop a fever over 100.4°F (38°C)
• start bleeding like a menstrual period or (and) are changing a pad every hour
• have severe pain in your abdomen or pelvis that the pain medication is not helping
• have heavy vaginal discharge with a bad odor
• have nausea and vomiting
• have chest pain or difficulty breathing
• leak fluid or blood from the incision or if the incision opens
• develop swelling, redness, or pain in your legs
• develop a rash
• have pain with urination
Caring for your incision:
• Your incision will be closed with either stitches or biological glue and covered with band-aids or a small dressing. You can remove the band-aids or dressing 24 hours after surgery. The stitches or glue will dissolve with time.
• If steri-strips are used, leave them on until they start to curl up on the edges (1 week)
• Keep your incisions dry for 24 hours.
Diet: You will continue with your regular diet.
Medications:
• Pain: Medication for pain will be prescribed for you after surgery. Do not take it more frequently than instructed.
• Stool softener: Narcotic pain medications may cause constipation. A stool softener may be needed while taking these medications.
• Nausea: Anti-nausea medication is not typically prescribed. Tell your doctor if you have a history of severe nausea with general anesthesia.
Activities:
• Energy level: It is normal to have a decreased energy level after surgery. During the first week at home, you should minimize any strenuous activity. Once you settle into a normal routine at home, you will slowly begin to feel better. Walking around the house and taking short walks outside can help you get back to your normal energy level more quickly.
Showers: Showers are allowed within 24 hours after your surgery. Do not take baths for at least 1 week after surgery.
Climbing: Climbing stairs is permitted, but you may require some assistance initially.
Lifting: For 2 weeks after your surgery you should not lift anything heavier than a gallon of milk. This includes pushing objects such as a vacuum cleaner and vigorous exercise.
Driving: The reason you are asked not to drive after surgery is because you may be prescribed pain medications. Even after you stop taking –pain medication; driving is restricted because you may not be able to make sudden movements due to discomforts from surgery.
Exercise: Exercise is important for a healthy lifestyle. You may begin normal physical activity within hours of surgery. Start with short walks and gradually increase the distance and length of time that you walk.To allow your body time to heal, you should not return to a more difficult exercise routine for 2 weeks after your surgery. Please talk to your doctor about when you can start exercising again.
Intercourse: No sexual activity for 2 weeks after surgery.
Work: Most patients can return to work between 1-2 weeks after surgery. You may continue to feel tired for a couple of weeks.
Other Symptoms:
• Vaginal Bleeding: Once your ovaries are removed you may have a period up to two weeks after your surgery.
• Menopausal Symptoms: Once your ovaries are removed you will be in surgical menopause. Symptoms of menopause may include hot flashes, vaginal dryness, mood changes, and vaginal discomfort with intercourse. If these symptoms cause you discomfort, please talk with your doctor.
Before the age of 45 there is a greater risk of thinning and broken bones after your ovaries are removed. It is important to get the right amount of calcium and vitamin D from your diet or a supplement. Your doctor may want you to have a bone density scan to evaluate your bone health.
