According to WHO, between 2 and 10% of couples worldwide are unable to conceive a child i.e. primary infertility and a further of 10-25% experience secondary Infertility i.e. are unable to conceive a second or subsequent child. Among these couples, infertility is exclusively a problem in the female in about 30-40% of cases, exclusively in the men in about 30-40% of cases and unexplained in 5-10% of couples. WHO believes that around 60-80 million couples in the world are infertile. The normal reproduction process requires interaction between the female and male reproductive tracts.
Infertility Management
Management of infertility includes both the physical and emotional care of couple. Types of fertility treatment available include:
• Medical treatment for lack of regular ovulation
• Surgical procedures, such as treatment for endometriosis, PCO drilling
• Assisted conception, which may be intrauterine insemination (IUI) or in-vitro fertilisation (IVF)
• Psychological support
Medical treatment of infertility generally involves the use of fertility medication, medical device, surgery, or a combination of the following. If the sperm are of good quality and the mechanics of the woman’s reproductive structures are good (patent fallopian tubes, no adhesions or scarring), Fertility doctor in India Dr.Samkar DasMahapatra may start by prescribing a course of ovarian stimulating medication.
Infertility specialist in India Dr.Mahapatra may also suggest intrauterine insemination (IUI), in which the Infertility doctor introduces sperm into the uterus during ovulation, via a catheter. In these methods, fertilization occurs inside the body.
Female Infertility tests:
Infertility, whether male or female, is defined as the inability of a couple to achieve conception or bring a pregnancy to term after a year or more of regular, unprotected sexual intercourse. For women over age 35, this condition is diagnosed after 6 months of an inability to conceive.
Fertility
Generally, The woman ovulates and releases an egg from her ovaries to travel through the fallopian tube to her uterus (womb). If any bloackage has been detected in the fallopian tube, infertility specialist in India will advise Fallopian tube block treatment in best infertility clinic in India. The male produces sperm. Both egg and sperm normally meet in the woman’s fallopian tube, where fertilization occurs. The embryo then implants in the uterus for further development.
Specific female causes Factors that can affect a woman’s chances of conceiving include being over- or underweight, or her age as female fertility declines sharply after the age of 35.
Common Causes Of Infertility In Females Include:
• Ovulation problems (e.g. polycystic ovarian syndrome)
• Tubal blockage
• Pelvic inflammatory disease
• Age-related factors
• Uterine problems
• Previous tubal ligation
• Endometriosis
• Advanced maternal age
Diagnosing and Treating Infertility with different tests and procedures:
Physical examination, both systemic and local
• Detection and timing of ovulation by basal body temperature (BBT), cervical mucus studies, ultrasonography, premenstrual endometrial biopsy and serum progesterone estimation in the mid-luteal phase.
• Assessment of tubal patency by appropriate investigations including hysterosalpingography, sonosalpingography, or laparoscopy
• Screening for local factors including cervical mucus-related problems and lower genital tract infections
• Assessment of uterine cavity by hysteroscopy.
• Screening for reproductive tract infections including syphilis, chlamydia, tuberculosis, HBV, HCV and HIV
• If needed, appropriate endocrinological investigations and therapy.
• Based on the results of these investigations, couples should be selected for treatment at different levels of infertility care units.
Male Infertility Test:
Many people think of infertility as a “woman’s problem,” although in about 40% of infertile couples, the man is the sole cause or a contributing cause of the inability to conceive. One-third of infertility cases can be attributed to male problems, including low sperm count. A visit to a urologist should start the evaluation for male infertility.
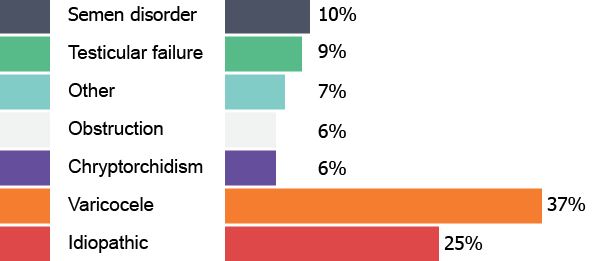
Specific Male Causes
The main cause of male infertility is low semen quality. Another possible cause is a low sperm count. Infertility associated with viable, but immmotile sperm may be caused by Primary Ciliary Dyskinesia. Other causes are, varicocele, scarring due to STDs ( gonorrhoea and Chlamydia), antisperm antibodies.
Male-fertility-test
• Physical examination, both systemic and local A good physical exam can detect varicoceles and give hints about hormonal problems.Testicular sizes are measured.
• Semen analysis including both morphological and functional tests The man’s sperm count, their shape, movement, and other variables are assessed through different tests.
• Screening for infections including syphilis, HBV, HCV and HIV
• If needed, appropriate endocrinological investigations and therapy like genetic tests which can identify specific obstacles to fertility.
Organising semen banking
Short-term semen cryobanking is the depositing, freezing and storage of sperm at a sperm bank for less than one year. Cryobanked sperm is then used in artificial insemination, in vitro fertilization (IVF) and other fertility treatment procedures.
Why cryopreserve Sperm
Some men discover they have diseases or must undergo treatment or surgery, which will cause permanent sterilization or genetic damage. As cancer detection and treatment techniques improve, more conditions such as cancer are being detected at younger ages in men, with longer survival rates. Therefore, more men in their fertile years are now considering cryopreservation to preserve their fertility after cancer diagnosis.
Fertility Surgery:
For some people, a structural problem can be treated through fertility promoting surgery in India. After initial assessment, Best fertility doctor in India Dr.Mahapatra recommends surgery – either to investigate the cause of infertility, or to treat problems that are making it difficult for you to conceive through best Infertility treatment in India.
Female Fertility Surgeries
Diagnostic Laparoscopy
• Usually performed as any day care procedure, under gen. anaesthesia and with minimal discomfort.
• Many infertile patients require laparoscopic surgery in infertility for a complete evaluation.
• It helps best fertility specialist in India Dr.Mahapatra to diagnose many problems including endometriosis, uterine fibroids and other structural abnormalities, ovarian cysts, adhesives, echopic pregnancy, tubal diseases and genital tuberculosis.
Diagnostic Hysteroscopy
• Diagnostic Hysteroscopy is used to examine the uterine cavity.
• It is an important tool in the study of infertility, recurrent miscarriages and abnormal uterine bleeding.
• It is helpful in diagnosing abnormal uterine conditions such as polyps, laternal fibroids, scaning adhesives and developmental abnormalities.
• For Infertility evaluation the hysteroscopy and laparoscopy are combined together usually soon after menstruation because uterine cavity is more easily evaluated & there is no risk of interrupting a pregnancy.
Operative Laparoscopy
• Many infertility disorders can be safely treated through the Laparoscopic surgery in India at the same sitting.
• Operating instruments like graspers, biopsy forceps, scissors, coagulators, electrosurgical or laser instruments, needle holders and suture materials are inserted through two or three incisions in the area above the pubis.
• Operative procedures include adhesiolysis, Laparoscopic surgery for endometriosis in India laparoscopic removal of chocolate cysts, Polycystic ovary syndrome & ovarian drilling in India, removal of diseased ovaries, uterine fibroids surgery in India, treatment of echopic pregnancy and treatment of blocked tubes or Hysteroscopic tubal cannulation in India.
• Laparoscopic tubal microsurgery is useful for tubotubal anastomosis, for reversal of sterilization, cornual anastomosis and diff salpingostomy for hydrosalpinges.
• Operations for female sterilization, hysterectomy, urinary incontinence and genital prolapse can also be performed laparoscopically.
• Endometriosis treatment in India involves surgical removal of the endometriosis and associated scar tissue.
• Laparoscopic ovarian drilling in resistant cases
Operative Hysteroscopy
• After dilating the cervix a hysteroscopy (a narrow telescope) is passed through the cervix into the uterine cavity.
• Special clear solutions (normal saline) are then injected into the uterus through the hysteroscope sheath. This disteuds the uterine cavity, clears blood and mucus and allows gynaecologist to directly view the inside of the uterus.
• A wider Hysteroscope allows operating instruments such as scissors, biopsy forceps, graspers, electrosurgical or laser instruments to be introduced into the uterine cavity through a channel in the operative hysteroscope.
• Fibroids, polyps, adhesives can be removed from inside the uterus.
• Congenital abnormalities, such as uterine septum, can also be corrected through the hysteroscope.
• Proximal Tubal Blocks can also be treated by Hysteroscopic cannulation, which utilizes the trans route & avoids incisional surgery. Traditional H+ for proximal tubal block by tubocormunal anastwosis is tedious and an invasive surgical procedure without encouraging results.
Risks
• Serious complications of diagnostic & operative laparoscopy are rare. Allergic reactions & anaesthesia complications rarely occur.
• The major risk is damage to bowel, bladder, uterus, major blood vessels or other organs.
• Certain conditions may lucrate the risk of serious complications. These include precious abdominal surgery, presence of bowel or pelvic adhesives, severe endometriosis, obesity or excessive thinness.
• In experienced hands, the risks of injury is 2-3/1000 procedures.
• Complications of hysteroscopy are rare and seldom serious. perforation of the uterus is the most common complication but it usually heals on its own. Some complications related to the liquids used to distend the uterus include fluid overload, pulmonary edema, blood clotting problems and severe allergic reactions.
Recovery
After Laparoscopy surgery in infertility / Hysteroscopy the patient is allowed to rest for 2-4 hours to recover from the anaesthesia. She is allowed liquids after 4hours and soft diet in the evening. After one operation the patient may feel some discomfort.
• Mild Nausea from medication or anaesthesia.
• A sore throat if a breathing tube was used during anaesthesia.
• Pain in the shoulders from the gas used during laparoscopy.
• Pain at the site of incision.
• Discharge like menstrual flow for a few days.
• Most of these minor complaints go in a day or two after surgery.
Conclusions
Previously, diagnosing & treating gynaecological problems required major surgery and many days of hospitalization.
However, laparoscopy & hysteroscopy allows correction of these problems on an outpatient basis. The procedures decrease patient discomfort, significantly reduce recovery time and have minimal risks.
Male Fertility Surgeries
As part of the diagnosis process, men receive a complete evaluation, including a fertility history, physical exam, blood testing, and semen analysis.
As with female surgery, male microsurgery involves specialised operative techniques,and these procedures are used to obtain sperm that can be used with IVF and ICSI including the use of an operating microscope. Surgeons trained in microsurgery use these skills and techniques for the repair of very small structures, such as the tubes that carry sperm or when little or no sperm is found in the edpididymal tubes or in case of any scarring. MESA is performed when infertility is caused by blockage and TESE involves removal of a small piece of testicular tissue through an incision in the testes
Varicosele Repair
This surgery is performed when varicose viens around the testes have enlarged and possibly produced too much heat due to which the quality of sperms decreases. This procedure has to be done cautiously to avoid testicular damage.
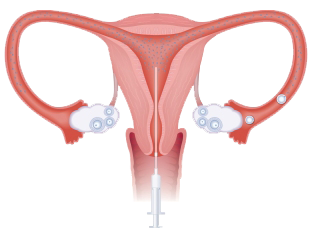
Intrauterine insemination (IUI):
Artificial insemination is often recommended in the setting of short-term unexplained infertility or sexual difficulties as an initial treatment before moving on to more complex fertility treatments such as in vitro fertilization (IVF). Fertility specialist doctor in India Dr.Sankar Das Mahapatra will recommend three to six treatment cycles depending on your particular circumstances before moving onto other treatment such as IVF. Infertility specialist Dr.Mahapatra may advise Artificial insemination technique used is known as intra uterine insemination (IUI) in India . It involves insemination of male partner’s (or donor) prepared sample through cervix to the cavity of the uterus at the time of Ovulation. This procedure can be performed during a natural cycle or with additional hormonal stimulation also called ovulation induction. The woman’s cycle is monitored to determine the day of ovulation. Once the follicle is mature, ovulation is triggered by an injection of synthetic human Chorionic gonadotropin (HCG). The prepared sperm is inserted directly into the uterine cavity using a very thin catheter.
Intrauterine insemination Guidelines for Semen Examination
• HIV, HBsAg for all IUI patients for both husband & wife.
• Sperm function test.
• More than 60 % live sperms than it’s a good sample.
• PH should be around 7.5.
Morphological Test
• HOS TEST (HYPO OSMOLAR SOLUTION TEST)
Staining Method:
• 1drp liq semen + 2 drp Eosin keep 30 seconds.add 3 drop of Nigrosin soln 10 sec.mix well. Make a thin smear. see under oil emulsion. If more than 50 % sperm stained than it is a bad sample.
• Clumping test for immunological infertility.
• 1 drp semen put cover slip see for clumping.
• If less motility add pinch of pentoxifylline powder.
• If liquefaction is poor add media add do repeated pipetting.
• If low count sends to JTS/SMM ask for collecting the 1st portion of ejaculation.
• If count good do IUI 24hrs after HCG and 38 hrs after HCG.
Stimulation Guidelines
• Clomiphene citrate from D2 To D6.
• Inj HMG 75 IU on D3 & D7.
• E 2 level on 10th day.
• Endometrium should be more than 8 mm. before giving HCG.
Special Cases
• Use of Eltoxin & Bromocriptine in selected cases.
• Use of metformine in patients of PCOD with post lunch insulin 3 times that of fasting insulin.
• Patients with high LH level use pure FSH instead of HMG.
• In resistance cases HMG to be started in higher doses from D 2